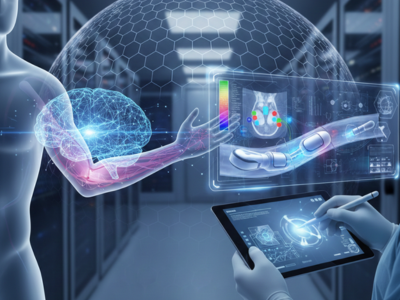
AI & Advanced Imaging Transform Lymphedema Diagnostics
Lymphedema diagnostics have evolved dramatically with advances in artificial intelligence (AI) and modern imaging technologies. Traditionally, clinicians relied on physical examinations and patient-reported symptoms to identify lymphedema, a condition where lymphatic fluid accumulates, causing swelling in the limbs. While these conventional methods remain important, they often fail to detect early-stage lymphedema. Therefore, accurate and timely lymphedema diagnostics are crucial for preventing disease progression, enhancing patient outcomes, and supporting personalized care.
Understanding Lymphedema
Lymphedema occurs when the lymphatic system cannot effectively drain lymphatic fluid, resulting in swelling, heaviness, and discomfort in the affected limbs. Early symptoms are subtle, including tightness, minor swelling, and skin changes. Patients often ignore these signs, leading to delayed diagnosis and complications.
Causes of Lymphedema
The condition can develop after cancer treatments such as lymph node removal or radiation therapy. Trauma, infections, and congenital abnormalities of the lymphatic system are also potential causes. Since lymphedema can severely affect mobility and quality of life, early and precise lymphedema diagnostics are essential to guide intervention strategies and prevent chronic complications.
Advanced Imaging in Lymphedema Diagnostics
Traditional Imaging Techniques
MRI (Magnetic Resonance Imaging), CT (Computed Tomography), and ultrasound are standard imaging modalities used to evaluate lymphatic structures. MRI provides high-resolution, three-dimensional imaging that helps detect deep tissue changes. Ultrasound offers real-time assessment of lymphatic flow and identifies obstructions causing fluid accumulation. These imaging methods complement physical examinations, improving the accuracy of lymphedema diagnostics and enabling clinicians to differentiate it from other causes of swelling, such as venous insufficiency.
Lymphoscintigraphy and Near-Infrared Fluorescence (NIRF)
Lymphoscintigraphy involves injecting a radioactive tracer into the limb, which travels through lymphatic vessels, highlighting blockages and dysfunction. NIRF imaging uses indocyanine green dye and infrared light to visualize lymphatic flow dynamically. This advanced technique is particularly effective in detecting early-stage lymphatic abnormalities before visible swelling appears. Together, these technologies significantly enhance the accuracy and depth of lymphedema diagnostics.
Artificial Intelligence in Lymphedema Diagnostics
AI-Powered Image Analysis
AI and machine learning are transforming lymphedema diagnostics by analyzing complex imaging data rapidly and consistently. Convolutional neural networks (CNNs) have been trained to classify images of swollen limbs, distinguishing lymphedema from conditions like deep vein thrombosis or chronic venous insufficiency. This approach reduces human error, accelerates diagnosis, and supports earlier interventions.
Quantitative Imaging and Disease Monitoring
AI also enables quantitative analysis of tissue changes, including automated segmentation and volumetric measurement. By tracking subtle changes over time, clinicians can monitor disease progression and evaluate treatment effectiveness with precision. The integration of AI into imaging workflows enhances reproducibility, facilitates personalized care, and provides objective metrics that guide clinical decisions.
Non-Invasive Diagnostic Tools
Bioimpedance Spectroscopy (BIS)
Bioimpedance spectroscopy measures the electrical resistance of tissues to detect fluid accumulation. When paired with AI algorithms, BIS can identify early lymphatic abnormalities months before swelling becomes clinically evident. Early detection using BIS allows for timely intervention, reducing the need for intensive therapies and improving long-term outcomes.
Wearable and Remote Monitoring Devices
Wearable technologies equipped with AI algorithms offer continuous monitoring of limb fluid changes. These remote diagnostics enable patients and clinicians to detect early signs of lymphatic dysfunction, supporting proactive management and reducing the likelihood of chronic complications. Such devices are increasingly important in modern lymphedema diagnostics, as they expand access to monitoring outside clinical settings.
Benefits of Advanced Lymphedema Diagnostics
Advanced diagnostic approaches offer several benefits:
- Early Detection: Identify lymphatic abnormalities before visible swelling occurs.
- Improved Accuracy: AI-enhanced imaging provides a precise assessment.
- Personalized Care: Data-driven insights guide individualized treatment plans.
- Continuous Monitoring: Wearables and remote devices facilitate proactive management.
- Reduced Complications: Timely intervention prevents disease progression and improves mobility.
These benefits collectively improve patient quality of life and support clinicians in delivering more effective care.
Challenges and Considerations
Despite these advances, challenges remain. MRI and CT scans are costly and may not be accessible in all regions. Ultrasound is operator-dependent, and AI algorithms require large, high-quality datasets to perform accurately. Additionally, clinicians must integrate these advanced diagnostics with traditional methods for comprehensive evaluation. Understanding the limitations and proper application of each tool ensures reliable and safe lymphedema diagnostics.
Future Perspectives
The future of lymphedema diagnostics lies in further integration of AI, imaging, and digital health. Continuous monitoring through wearables, combined with predictive analytics, will allow clinicians to detect lymphatic dysfunction earlier and provide tailored interventions. Advanced biomarkers and AI-assisted imaging will refine risk stratification models, enabling proactive surveillance for high-risk individuals. These innovations promise more efficient, personalized, and precise care for patients with lymphedema.
Conclusion
AI and advanced imaging have transformed lymphedema diagnostics by providing faster, more accurate, and personalized assessments. These tools complement traditional clinical evaluation, enabling early detection, better treatment planning, and improved patient outcomes. By integrating AI, imaging technologies, and non-invasive monitoring, clinicians can intervene proactively, reducing chronic swelling, improving mobility, and enhancing quality of life. Modern lymphedema diagnostics are not just tools—they represent a paradigm shift in patient-centered lymphatic care.